Social Risk Adjustment initiative provides funds to physician organizations to help them address social factors that impact patients’ health
Mary has missed her last four doctor appointments because she lacked transportation to get there. John tries to make healthy meals, but he doesn’t live near any stores that sell fresh produce. Nancy isn’t sure she’s taking her medications properly, because she has a low reading level and doesn’t understand the directions. For each of these patients, social, not clinical, factors affect their ability to access, receive or follow-through on needed health care. These social determinants of health can affect a person’s health outcomes more than the care provided in a clinical setting.
With this in mind, Blue Cross Blue Shield of Michigan launched a new social risk adjustment initiative, providing funds to physician organizations so they can address specific needs unique to the communities where their practices are located. The initiative is part of the Physician Group Incentive Program.
“The initiative supports physician organizations caring for patients with high levels of social needs affecting their overall health. It uses the Area Deprivation Index to identify members who are at the highest risk for poor health outcomes,” said David Bye, clinical program development manager at Blue Cross. “The ADI uses 17 variables to rank neighborhood areas from 1 to 10, with 10 representing the most disadvantaged areas.”
Some of these variables include:
- Housing quality and stability
- Access to transportation
- Ability to afford and purchase quality food
- Ability to afford health care
- Social support system
- Community safety
- Education and employment status
Patients with socially complex issues often use more health care services than others. Addressing the social determinants can require care teams to spend extra time and resources. Directing payments to providers who care for more socially disadvantaged patients will provide additional resources to help in closing social need gaps.
About ADI
The ADI is based on a measure created by the Health Resources & Services Administration* more than three decades ago, and has since been refined, adapted and validated by a team at the University of Wisconsin-Madison.
The map below from the university’s Neighborhood Atlas® website* shows the ADI scores for Michigan. Red indicates the most disadvantaged areas. The scores measure an area’s degree of social risk to residents down to the neighborhood block level since social needs can vary greatly from block to block.
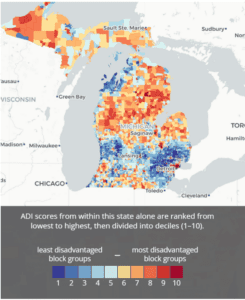
“Many studies show that patients experience a gradual worsening of various outcomes as the ADI level where they live increases,” said Marti Walsh, M.D., senior medical director and associate chief medical officer for Blue Cross. “Patients in higher ADI areas are shown to have worse health outcomes. Our goal is to provide some funding to help address these needs and improve outcomes.”
For purposes of this initiative, each physician organization will be evaluated for members who have an ADI of 8 or above. Organizations will receive funding based on the number of members they have in this higher ADI range. The funding is to be used to address the specific needs of their patient population, including transportation and food instability.
During this initial phase of the initiative, organizations that opt in will complete a brief survey to collect status updates on the use of the funding. They’ll also begin participating in sessions to share best practices with their peers.
“This is an incredibly valuable initiative, and we anticipate it will positively impact our members,” said Dr. Walsh. “It aligns with the Blue Cross social mission to make affordable, high-quality health care accessible to everyone in Michigan.”



