Continuous Learning Through Peer Review Makes Angioplasty and Stenting Better in Michigan
By: Debbie Reinheimer

If you receive an angioplasty at a Michigan facility, you might take comfort in knowing that the team performing the procedure participates in a statewide quality improvement initiative called the BMC2. It’s also likely that the interventional cardiologists who perform the angioplasty have received feedback from their peers, helping them learn and share best practices and improve the angioplasty process.
Angioplasty and stenting is a common procedure used to widen or unblock coronary arteries and restore blood flow. Sometimes, an angioplasty is a planned procedure. Other times, an angioplasty may be performed urgently, such as when a patient is having a heart attack. Most angioplasty procedures are successful in the short term, but there are technical nuances that differentiate a good from an excellent procedure. A high quality procedure is more likely to result in a longer lasting result. That’s where this peer review process comes in.
“Physicians across the state review each other’s cases as a quality assurance check to assess the appropriateness and quality of the procedure. Operators receive scores and comments back from those who reviewed their cases,” said Hitinder Gurm, M.D., director of BMC2 . “It’s a great opportunity for all of us to share, learn and improve.”
Participating physicians say the feedback has been valuable, particularly because it comes from their peers – other interventional cardiologists who understand the complexities and clinical presentation of such a procedure.
More than 1,500 cases have been reviewed since the peer review effort began in 2017.
What really makes it work is that both the reviewers and the reviewees are anonymous. This removes any sense of competition or judgement and frees physicians to collaborate for the greater good of improving patient care.
Reviewers get case information, including medical record documentation and copies of angiograms to help them understand the case. The angiograms allow reviewers to see the actual procedure and how well the angioplasty was done. Patient information is de-identified in all cases.
“Reviewers consider not just the quality of the procedure, but also the appropriateness and best treatment for the patient. For example, they evaluate whether medical management or a surgical intervention would have been a more appropriate option for each case,” said Gurm.
When reviews are complete, the files are sent back to the BMC2 coordinating center. The coordinating center then creates a report that goes back to the hospital site being reviewed. Each hospital gets its own report.
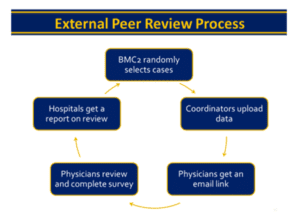
Using case identification numbers, hospitals can then match the case reviews with the physicians who performed the case and share the reviews back to them confidentially.
“The cross-site feedback has been valuable for all participants,” said Annemarie Forrest, M.S., MPH, R.N., program manager for BMC2. “Physicians appreciate the opportunity for continued learning from each other.”
The BMC2 began in 1997 as a way to share data and improve the quality of angioplasty procedures statewide. With information from more than 500,000 procedures collected from every Michigan facility where angioplasties are performed, the BMC2 registry offers a vast stockpile of data that physicians can use to improve the processes, safety, quality and outcomes of angioplasty procedures.
For more information, go to bmc2.org.


